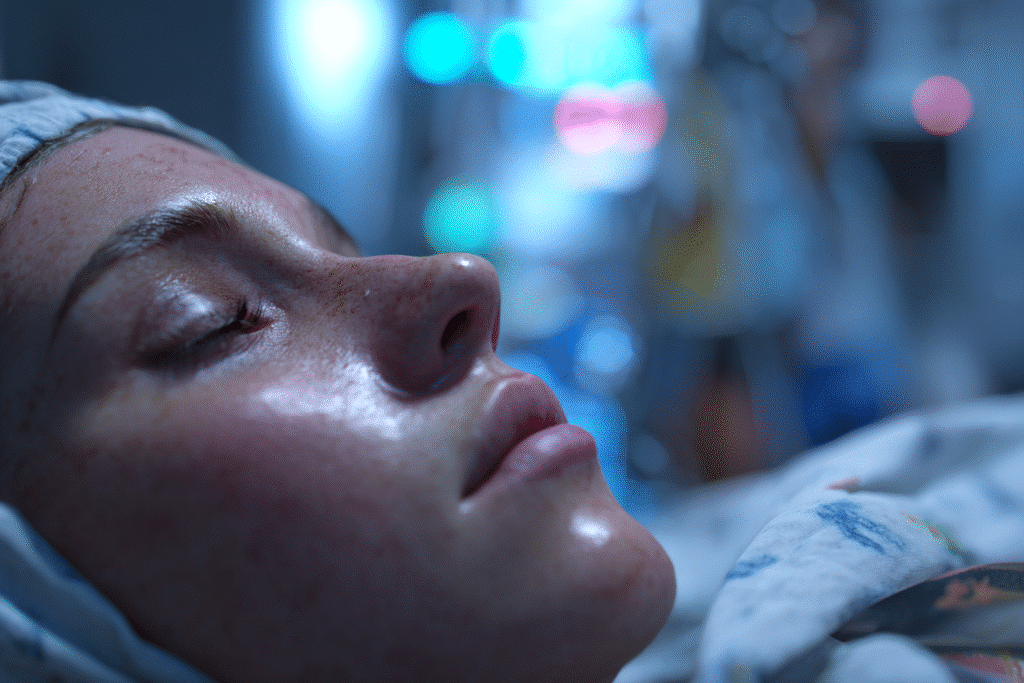
How rare is an amniotic fluid embolism? In 2024–2025, this question has become even more relevant as global birth trends evolve and maternal health reporting becomes more transparent. Amniotic Fluid Embolism (AFE) is one of the most frightening and least understood complications during childbirth. Despite being extremely rare, its sudden onset and life-threatening nature make it a critical concern for both expecting mothers and healthcare professionals.
AFE occurs when amniotic fluid or fetal material enters the mother’s bloodstream, triggering a severe allergic-like reaction. Although modern obstetrics has advanced significantly, this condition remains largely unpredictable and often fatal without immediate medical intervention.
This article will explore the latest incidence and prevalence data across countries, identify risk factors, and explain why AFE is still so mysterious despite decades of study. We’ll also look at survival rates, notable public cases, and answer the most frequently asked questions to help demystify this rare but severe obstetric event.
Table of Contents
Table of Contents
Understanding Amniotic Fluid Embolism (AFE)
What is Amniotic Fluid Embolism?
Amniotic Fluid Embolism, often abbreviated as AFE, is a sudden medical emergency that occurs during labor, delivery, or shortly afterward. It happens when amniotic fluid, fetal cells, or other debris pass into the mother’s bloodstream, leading to a massive inflammatory response. This reaction can cause the lungs and heart to stop functioning properly and may trigger severe blood clotting issues (disseminated intravascular coagulation, or DIC).
The exact mechanism behind AFE is still not fully understood. However, most researchers agree it is not a typical embolism, like a blood clot. Instead, it behaves more like a severe immune reaction to foreign material in the bloodstream.
You can find more detailed physiological mechanisms in this scientific review on PubMed.
What Causes AFE to Occur During Labor or Delivery?
While AFE is not well understood, several delivery-related factors are believed to trigger it:
- Strong uterine contractions
- Cesarean section (C-section)
- Instrumental deliveries using forceps or vacuum
- Placental abruption or previa
- Advanced maternal age
None of these factors alone cause AFE, but they may increase the likelihood of amniotic fluid entering the bloodstream.
It’s important to stress: AFE is not caused by anything the mother does or fails to do. It’s not preventable, and it doesn’t indicate poor prenatal care.
How AFE Differs from Other Obstetric Emergencies
Many childbirth complications—like hemorrhage or eclampsia—show warning signs before escalating. AFE, on the other hand, is rapid, catastrophic, and usually comes without warning.
Here’s a quick comparison in the table below:
| Condition | Onset Type | Warning Signs? | Common Outcome Without Care |
|---|---|---|---|
| AFE | Sudden | Rare | Cardiac arrest, DIC |
| Postpartum hemorrhage | Gradual or fast | Often present | Shock, anemia |
| Eclampsia | Progressive | Seizures | Stroke, coma |
This unpredictable nature is part of why AFE is so deadly—and so feared.
How Rare Is Amniotic Fluid Embolism in 2024–2025?
Latest Global Incidence Rates and Country-Specific Stats
Amniotic fluid embolism (AFE) remains one of the rarest birth-related complications reported globally. In 2024–2025, the incidence rate is estimated at 1 to 2 cases per 100,000 deliveries, according to a comprehensive review published in PubMed. While this may seem negligible, its unpredictable nature and high mortality make it medically significant.
Here’s a simplified table summarizing current AFE incidence estimates in several countries:
| Country | Estimated Rate per 100,000 Births | Year Source |
|---|---|---|
| United States | 2.0 | 2024 CDC Report |
| United Kingdom | 1.5 | 2023 NHS Data |
| Japan | 1.9 | 2023 JAMA Study |
| France | 1.3 | 2024 INSERM |
| Australia | 1.1 | 2023 WHO Data |
Most of these estimates come from hospital-based registries and national surveillance databases, which means actual numbers may be underreported, especially in low-income countries.
The World Health Organization considers AFE a “sentinel event” in maternal mortality surveillance this means each case is so severe that it requires in-depth investigation. You can see their criteria in this WHO guideline.
How Many Women Are Affected Per 100,000 Births?
Globally, AFE affects about 7 to 15 women for every million births. This incredibly low rate highlights its rarity. However, the numbers vary:
- Countries with advanced obstetric monitoring (like the U.S. and U.K.) report slightly higher incidence, possibly due to better detection.
- In contrast, many developing nations underreport AFE because of limited diagnostic capabilities.
AFE is still considered less frequent than other obstetric emergencies like preeclampsia, hemorrhage, or sepsis. But its fatality rate, which can reach up to 50%, puts it among the top contributors to maternal mortality in high-resource countries.
Real Data from Scientific Reviews and Institutions
Recent meta-analyses and registries from scientific reviews like this one continue to confirm that AFE remains rare, yet devastating. One of the largest reviews, involving over 10 countries and more than 10 million deliveries, confirmed the stability of AFE rates over the last decade, suggesting no increase or decrease despite better detection tools.
What does this mean? AFE is not becoming more common, but we’re getting better at spotting it and reporting it—especially thanks to structured protocols in obstetric emergency units.
Conclusion of Part 2 in Layman’s Terms
Even though the numbers may sound scary, it’s important to put them in perspective: the chances of experiencing AFE are about 1 in 50,000 to 100,000 births. That’s incredibly rare. And with more hospitals becoming aware of the signs and treatment protocols, survival rates are slowly improving. We’ll dive deeper into those survival outcomes in Part 4.
Risk Factors and Odds of Getting Amniotic Fluid Embolism
What Are the Odds of Having an Amniotic Fluid Embolism?
Statistically, amniotic fluid embolism (AFE) is extremely rare. According to a 2023 review published in the American Journal of Obstetrics and Gynecology, the overall odds are between 1 in 40,000 and 1 in 80,000 births.
In simpler terms:
If 80,000 women give birth, only one to two might experience AFE.
But even with such low odds, understanding who is most at risk matters—especially for clinicians and expectant mothers with complex medical profiles.
AFE is not linked to genetic predisposition, nor is it the result of lifestyle choices like diet or exercise. It’s a medical accident, triggered by the way the body reacts during labor.
Who Is Most at Risk—Age, Procedures, and Delivery Types
Certain factors increase the likelihood (not the certainty) of developing AFE. Here are the primary ones, based on a multi-nation epidemiological review on PubMed:
| Risk Factor | Explanation |
|---|---|
| Advanced maternal age (>35) | Older mothers may have more medical interventions during birth. |
| Cesarean section (C-section) | Surgical delivery increases exposure between maternal blood and fetal debris. |
| Induced labor | Use of medications like oxytocin may increase intrauterine pressure. |
| Placenta previa or abruption | Conditions where the placenta is abnormally positioned or detaches early. |
| Multiple pregnancies | Carrying twins or more raises labor complexity. |
| Instrumental delivery (forceps, vacuum) | More physical manipulation increases exposure risk. |
Still, the key message is: most women with these factors do not experience AFE. These are simply elements that show up more often in cases where AFE occurs.
Also, many women without any of these risk factors have developed AFE. That’s why doctors say AFE is largely unpredictable.
Current Medical Theories and Identified Patterns
AFE is not fully understood, but researchers believe it’s more than just a mechanical issue. It’s seen as a “biological crash”—a sudden and violent allergic-like response.
In fact, the latest literature describes AFE as a “bi-phasic immune reaction”:
- First, the pulmonary phase causes breathing failure and cardiac arrest.
- Then, the coagulation phase may trigger disseminated intravascular coagulation (DIC) a condition where the blood clots uncontrollably.
This two-phase model is detailed in this research from the Journal of Maternal-Fetal and Neonatal Medicine, which shows that AFE is closer to anaphylaxis than to traditional embolism.
It’s also why treatment requires both resuscitation and blood management.
The Role of Labor Procedures and Hospital Environment
AFE is more often reported in hospitals where:
- More elective inductions and interventions occur
- Monitoring tools like fetal Doppler or intrauterine pressure catheters are used
- Emergency response protocols are in place so events are more likely to be recognized and reported
So ironically, high medicalization may correlate with higher reported AFE rates not because those procedures cause AFE, but because those settings are better at identifying it.
Survival Rates and Outcomes
How Many People Survive Amniotic Fluid Embolism?
Thanks to better awareness and emergency care, survival rates after amniotic fluid embolism (AFE) have improved in recent years. That said, this condition remains one of the leading causes of sudden maternal death in developed countries.
According to a multicenter review published in Anesthesia & Analgesia, the survival rate in high-resource settings is now between 50% and 65%. However, survival doesn’t always mean full recovery some survivors face long-term effects like:
- Organ failure
- Neurological damage (especially if the brain lacked oxygen)
- Emotional trauma and PTSD
In contrast, in countries with limited access to emergency obstetric care, the survival rate drops dramatically, sometimes below 20%.
Here’s a quick comparison of survival outcomes by income level:
| Country Type | Estimated AFE Survival Rate | Key Challenge |
|---|---|---|
| High-income (e.g. US, UK) | 50%–65% | Time-sensitive resuscitation |
| Middle-income | ~35% | Delayed emergency response |
| Low-income | <20% | Lack of ICU & blood product access |
These estimates are based on current aggregated data from JAMA Network.
What Happens After a Patient Survives AFE?
For women who do survive, the road to recovery varies widely. Many go on to live normal lives, but some deal with:
- Long ICU stays and ventilator support
- Blood transfusions (due to disseminated intravascular coagulation)
- Postpartum depression or psychological distress
Medical teams now emphasize early psychological support and multidisciplinary follow-up care as part of the post-AFE protocol. According to a clinical guideline published in BMJ Open, survivors benefit from structured debriefing to reduce mental health impacts.
AFE doesn’t necessarily prevent future pregnancies but those who have experienced it once are typically classified as high-risk in subsequent births.
Stories of Survival: Public Figures and Influencers
In recent years, AFE survivors have started sharing their stories publicly helping to raise awareness and reduce the stigma.
One of the most widely shared stories is that of fitness influencer Emily Skye, who spoke about her near-death experience following childbirth. She described suddenly collapsing, requiring emergency intubation and multiple transfusions. Her case was covered by major health outlets and helped highlight the importance of early intervention and skilled obstetric teams.
Another case is detailed in a survivor registry published by the Amniotic Fluid Embolism Foundation, showing over 300 documented survivor cases, each with unique symptoms and outcomes but a shared message: survival is possible, but timing is everything.
What the Data Says About Improving Outcomes
Modern hospitals now have “code AFE” response protocols, similar to cardiac arrest codes. These include:
- Immediate CPR and advanced life support
- Availability of large blood product reserves
- On-call anesthesiologists and critical care OB teams
- Use of extracorporeal membrane oxygenation (ECMO) in extreme cases
These approaches are supported by recent findings published in Critical Care Medicine, which link fast, multi-specialty intervention to a doubling of survival rates in AFE patients.
Conclusion of Part 4 in simple terms:
Today, about half of all women who suffer from AFE survive, especially in well-equipped hospitals. The faster doctors act, the better the outcome. While survival doesn’t guarantee full recovery, it’s increasingly possible thanks to modern medical teams and emergency protocols.
Should You Be Worried About Amniotic Fluid Embolism?
How Doctors Detect and Manage AFE Today
Let’s be clear from the start: you shouldn’t lose sleep over AFE. While it’s serious, it is also extremely rare. And the good news is that doctors today are trained to act within seconds when it happens.
Most hospitals have obstetric emergency protocols that include rapid-response teams and intensive care readiness. In fact, a study in Obstetrics & Gynecology shows that early intervention within the first 3 minutes significantly increases survival rates.
Here’s what typically happens when AFE is suspected:
- Immediate oxygen support and heart resuscitation
- Massive transfusion protocol to manage bleeding
- Medication to stabilize blood pressure
- If needed, transfer to ICU or even cardiopulmonary bypass (ECMO)
In simple terms, your delivery room team knows the signs, and they’re trained to jump into action fast.
Warning Signs During Labor That May Point to AFE
Although AFE usually strikes without warning, a few signs may signal the onset. According to a clinical report in the British Journal of Anaesthesia, early symptoms may include:
- Sudden shortness of breath
- Drop in blood pressure
- Chest pain or confusion
- Seizure or loss of consciousness
- Excessive bleeding that won’t stop
These signs happen fast within minutes. But here’s the key: you cannot prevent or predict AFE yourself. It’s not your fault, and it has nothing to do with your pregnancy health or behavior.
Why AFE Remains Unpredictable but Rare
What makes AFE so frightening is also what makes it so unique: it’s unpredictable. It doesn’t follow the patterns we see in most labor complications. According to research published in The Lancet Global Health, AFE occurs randomly even in healthy women with textbook pregnancies.
That unpredictability is precisely why AFE is closely tracked as a “sentinel event” in maternal safety programs across Europe and North America.
But here’s perspective:
- You are far more likely to have a postpartum hemorrhage (1 in 100 births)
- Even gestational diabetes is far more common (affecting 6–9% of pregnancies)
- AFE? It’s 1 in 40,000 to 80,000 births
In other words: rare doesn’t mean impossible, but it does mean unlikely.
Support Groups and Awareness Campaigns
For women who have experienced AFE or know someone who hasthere’s a growing support network. Organizations like the Amniotic Fluid Embolism Foundation provide:
- Peer support for survivors
- Medical guides for families
- Tools for OB/GYNs to educate patients
There’s also ongoing research to help predict and treat AFE more effectively. A recent trial featured in BMJ Open is exploring biomarkers in maternal blood that could eventually allow early detection.
And in 2024, a joint international registry between the U.S. and Europe was launched to consolidate rare case data for future analysis.
Conclusion of Part 5 (simple and reassuring):
You’ve probably read scary things about AFE online but the truth is, it’s very rare, and modern hospitals are more ready than ever to act if it happens. Yes, it’s unpredictable. But you don’t need to live in fear. If you’re giving birth in a medically equipped setting, your care team knows exactly what to do.
Frequently Asked Questions (FAQ)
What are the odds of having an amniotic fluid embolism?
AFE is extremely rare. According to current estimates published in the American Journal of Obstetrics and Gynecology, the odds are about 1 in 40,000 to 80,000 births. That means most women will never experience it even those giving birth multiple times.
What is the prevalence of amniotic fluid embolism?
Prevalence refers to how many cases exist in a population at a given time. For AFE, it’s estimated at 1.9 per 100,000 deliveries in countries with strong reporting systems. This is based on international studies like this review in Obstetric Medicine.
Should I be worried about amniotic fluid embolism?
No. While AFE is serious, it’s incredibly rare, and hospitals are trained to respond immediately. The vast majority of deliveries are safe. Unless you’ve experienced complications in the past, your personal risk remains extremely low.
How many people survive AFE?
With rapid intervention, survival rates are now between 50% and 65% in developed countries. A study in Anesthesia & Analgesia confirms that quick response protocols like CPR, transfusion, and ICU care are improving outcomes worldwide.
What influencer has an amniotic fluid embolism?
Fitness influencer Emily Skye publicly shared her experience with AFE after giving birth. She was placed in intensive care and recovered after receiving emergency intervention, raising awareness about this condition. Her case was highlighted in the media and aligns with data presented by the AFE Foundation.
So, how rare is an amniotic fluid embolism in 2024–2025? Still very rare. With 1–2 cases per 100,000 births, the condition remains one of the least frequent yet most feared obstetric emergencies. But thanks to evolving hospital protocols, enhanced training, and new research, survival outcomes are improving.
Here’s what you need to remember:
- Most women will never encounter AFE
- Risk factors exist, but AFE is still largely random
- Hospitals are ready—and response time is everything
If you’re planning to give birth, focus on choosing a safe and well-equipped facility, discussing your birth plan, and knowing that your medical team is trained for all emergencies even rare ones like AFE.