Amniotic Fluid Embolism (AFE) is a rare but catastrophic complication that can strike without warning during labor, delivery, or immediately postpartum. While its exact cause remains elusive, what’s clear is that rapid identification and proper management can be the difference between life and death. In this article, we explore the most recent, evidence-based strategies for reducing the risk of AFE starting from the decision to induce labor, all the way to choosing whether to use vacuum or forceps during delivery.
Our goal is to offer practical guidance grounded in scientific literature and clinical experience, yet written in plain English for families, healthcare workers, doulas, and anyone navigating childbirth. Through this comprehensive guide, you’ll gain insights into risk reduction, safe delivery practices, and critical moments where intervention can make a life-saving impact.
Don’t miss our article on the risk factors of AFE if you want to dive deeper into causes.
Table of Contents
Table of Contents
Understanding Amniotic Fluid Embolism (AFE)
What is Amniotic Fluid Embolism and Why It’s So Dangerous
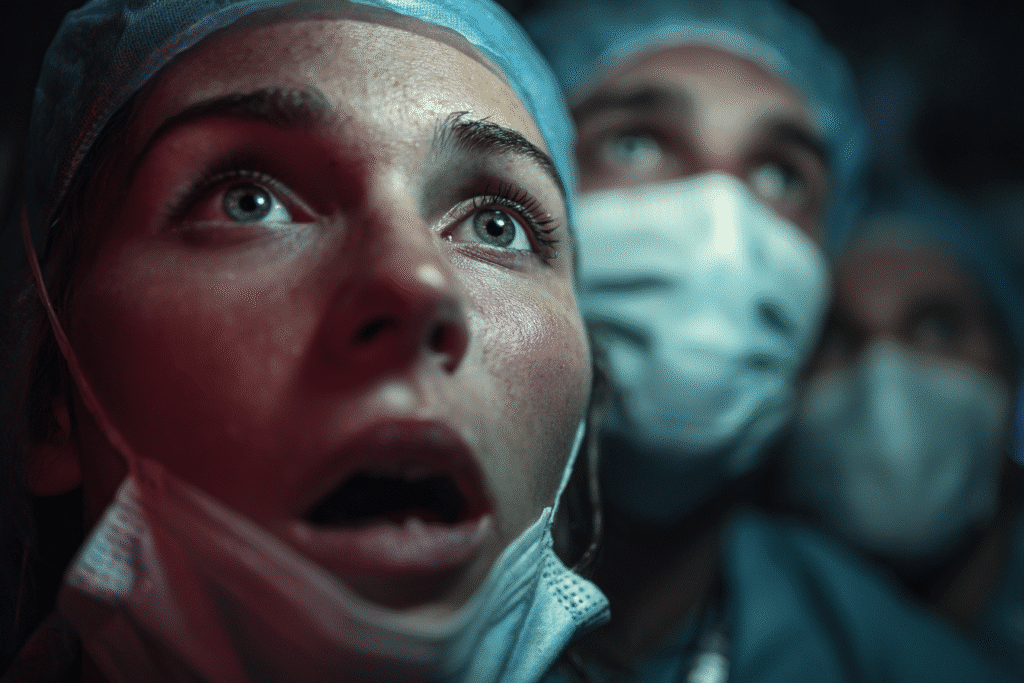
Amniotic Fluid Embolism, or AFE, happens when amniotic fluid or fetal material enters the mother’s bloodstream, usually during labor or delivery. This sets off a violent reaction: a chain of immune and cardiovascular breakdowns that can lead to heart failure, respiratory collapse, and coagulopathy (severe bleeding).
Unlike many complications, AFE is unpredictable and rapid. Once symptoms begin, a woman may lose consciousness, develop shortness of breath, or go into shock within minutes. That’s why AFE is often described as one of the most feared obstetric emergencies.
According to PubMed studies, survival hinges on swift recognition and coordinated emergency care.
But here’s the good news: while AFE is rare, its risk can be minimized by making informed decisions at every stage of labor.
Clinical Presentation and Early Warning Signs
Knowing the signs saves lives. AFE typically shows up in two phases:
- First Phase – Sudden Collapse:
- Shortness of breath
- Anxiety or confusion
- Drop in oxygen levels
- Seizure or cardiac arrest
- Second Phase – Coagulation Breakdown:
- Massive bleeding
- Inability of blood to clot
- Uterine atony (soft uterus unable to contract)
A sudden shift in a woman’s condition especially after rupture of membranes or delivery of the placenta should immediately raise red flags. Teams should initiate AFE-specific emergency protocols when such symptoms appear.
For a simple overview of these symptoms, check out the educational explainer on Amniotic Fluid Embolism.
Clinical guidelines from NIH recommend constant monitoring in high-risk patients and immediate access to advanced resuscitation equipment in labor wards.
Risk Factors: Who’s More Vulnerable?
Maternal, Fetal, and Procedural Risk Contributors
While Amniotic Fluid Embolism (AFE) strikes unpredictably, certain risk factors have been identified in large-scale obstetric reviews. Women over age 35, those carrying multiples (twins, triplets), or with abnormal placental conditions like placenta previa are statistically more vulnerable to developing AFE.
Clinical evidence from PubMed highlights that advanced maternal age, polyhydramnios (excess amniotic fluid), and cesarean delivery significantly increase AFE incidence. Additionally, a prior uterine surgery, such as a myomectomy or cesarean, can compromise uterine integrity, allowing fetal cells to more easily enter the bloodstream during delivery.
A comprehensive list of maternal risk factors includes:
| Maternal Factors | Fetal/Placental Factors | Procedural Factors |
|---|---|---|
| Age > 35 | Multiple gestation | Induction of labor |
| Obesity | Macrosomia (large baby) | Cesarean section |
| Preeclampsia | Placental abruption | Intrauterine pressure catheter use |
| Prior uterine surgery | Polyhydramnios | Uterine rupture |
Importantly, not all women with these factors will develop AFE. However, their presence should guide decisions about labor induction and monitoring, especially in facilities without immediate access to advanced critical care.
For a more detailed analysis of AFE risk variables, review the internal article on Amniotic Fluid Embolism Risk Factors.
Common Triggers During Labor & Delivery
AFE usually occurs during or immediately after labor. Certain medical interventions, while necessary in many births, are statistically associated with higher AFE risk. For instance, induction with uterotonic agents like oxytocin can cause uterine hyperstimulation, increasing intrauterine pressure and potentially forcing amniotic fluid into the bloodstream — a pathophysiological trigger well-documented in clinical research.
Other potential triggers include:
- Artificial rupture of membranes (especially when combined with internal monitors)
- Forceps or vacuum-assisted deliveries, which can cause microtears in the cervix or uterus
- Cesarean deliveries under emergency conditions
- Intrauterine pressure catheters, shown in this NCBI study, can introduce fetal material directly into maternal vessels
Notably, a case-controlled study on AFE published by the American Journal of Obstetrics and Gynecology found that trauma to the uterine wall was a recurring theme in over 60% of AFE events.
Reducing the number of interventions and choosing evidence-backed induction methods can go a long way in preventing unexpected complications like AFE especially in high-risk cases.
Decision-Making Around Induction: Minimizing AFE Triggers
Elective vs Medically-Indicated Induction
The decision to induce labor should never be taken lightly, especially when considering the risk of Amniotic Fluid Embolism. There’s a growing trend toward elective inductions scheduling labor for non-medical reasons like convenience or provider preference but this carries unintended risks.
According to a comprehensive review from PubMed, elective inductions before 39 weeks have been associated with increased maternal morbidity, including rare events like AFE. Medical induction, on the other hand, is typically recommended when continuing the pregnancy poses greater risk than delivering for example, in preeclampsia or fetal growth restriction.
Here’s a simple comparison:
| Type of Induction | Common Reasons | AFE Risk Impact |
|---|---|---|
| Elective | Personal schedule, maternal request | Slightly increased due to unnecessary intervention |
| Medically-Indicated | Preeclampsia, fetal distress, post-term | Lower risk if appropriately timed |
Ultimately, timing matters. When induction is warranted, choosing the safest method becomes the next critical step in minimizing AFE risk.
Cervical Ripening Agents: Are Some Safer Than Others?
The choice of medications or techniques to soften the cervix (cervical ripening) has been shown to influence uterine activity and in some cases, the potential to trigger AFE.
Prostaglandins (like misoprostol and dinoprostone), oxytocin (Pitocin), and mechanical dilation methods (balloon catheters) are commonly used. But not all of them are equal in safety profiles.
Research from NCBI shows that hyperstimulation of the uterus more than 5 contractions in 10 minutes can lead to increased pressure in the amniotic sac. This can push fetal cells into the bloodstream, potentially initiating the immune cascade seen in AFE. Uterine hypertonus, particularly when combining agents like prostaglandins and oxytocin, is a known red flag.
A clinical breakdown of common ripening methods:
| Method | AFE Risk Factor | Notes |
|---|---|---|
| Misoprostol (Cytotec) | Moderate (especially when overdosed) | Avoid multiple doses closely timed |
| Oxytocin (Pitocin) | High when used without monitoring | Always combine with fetal monitoring |
| Balloon catheter | Lower | Preferred for high-risk pregnancies |
Clinical protocols now recommend starting with mechanical methods when possible in patients with known risk factors for AFE. It’s also crucial to avoid overlapping high-dose uterotonics.
For evidence-based insights on medication-induced complications and AFE risk, refer to this systematic review on uterotonic safety.
Additionally, your internal guide on causes and prevention of AFE offers a patient-friendly breakdown of these same concerns.
Making induction decisions guided by risk stratification, clinical evidence, and multidisciplinary planning is essential for improving outcomes.
Delivery Setting: Hospital vs Home Birth Considerations
Emergency Preparedness in Delivery Settings
When it comes to preventing Amniotic Fluid Embolism, where a woman gives birth matters almost as much as how. The critical difference lies in the ability to respond within seconds if AFE strikes and that response window is incredibly narrow.
Hospitals are equipped with rapid-response teams, blood transfusion units, and intensive care support that simply aren’t available in a home setting. AFE often presents without warning, and immediate access to advanced resuscitation, intubation, and cardiopulmonary support is crucial to survival, as shown in this PubMed clinical analysis.
According to the American College of Obstetricians and Gynecologists, even well-planned home births carry a higher risk of poor neonatal and maternal outcomes in the event of unexpected emergencies. AFE, by nature, does not give anyone time to transport the patient to safety.
Here’s a quick comparison of delivery settings:
| Factor | Hospital Birth | Home Birth |
|---|---|---|
| Resuscitation Equipment | Fully equipped (ventilators, ICU) | Limited to basic tools |
| Blood Transfusion Availability | Immediate | Not available on-site |
| Surgical Team Access | 24/7 coverage | Not available |
| Neonatal Intensive Care Unit | On standby | Requires transport |
| AFE Response Capability | High survival potential | Critically delayed |
The takeaway? If a patient is already at risk for AFE, or any pregnancy complication, delivering in a hospital isn’t just safer — it’s life-saving.
Explore this in-depth article on AFE and home birth for more details on why setting matters.
Why Home Birth May Increase AFE Risk
Advocates of home birth often highlight the natural, low-intervention environment, but when it comes to rare but catastrophic events like AFE, the absence of immediate medical intervention can be devastating.
AFE can lead to cardiopulmonary collapse and DIC (disseminated intravascular coagulation) within minutes. That means every second counts, and even a five-minute transport delay can result in irreversible damage or death, as emphasized in this study on emergency obstetric outcomes outside hospitals.
While not all home births are unsafe, those involving:
- VBACs (vaginal birth after cesarean)
- Multiples
- Preeclampsia or gestational hypertension
- Overdue pregnancies with meconium-stained fluid
carry an elevated risk for sudden complications, including AFE. These scenarios are better managed in settings with emergency backup not just a midwife and an oxygen tank.
Moreover, cases have been reported where AFE was mistaken for maternal anxiety or syncope in home births, leading to delayed or incorrect treatment.
It’s not about fear it’s about preparedness. For high-risk patients, clinical safety must override birth plan preferences when the stakes involve a condition as fatal as AFE.
Dive deeper into how rare AFE really is to understand its unpredictable nature and how delivery settings impact survival odds.
Monitoring During Labor: Preventive Protocols That Matter
Continuous Fetal Monitoring and Its Role
One of the most effective strategies to prevent Amniotic Fluid Embolism-related fatalities is early detection of abnormal changes in the mother’s or baby’s condition. This is where continuous monitoring both maternal and fetal becomes non-negotiable.
AFE often presents with a sudden drop in oxygen saturation, fetal distress, or cardiovascular collapse. These signs may appear as subtle anomalies on the fetal heart rate monitor or as abnormal maternal vital signs.
A review published on PubMed emphasizes that in nearly 90% of AFE cases, fetal bradycardia (low heart rate) was the first visible indicator often occurring just before maternal symptoms emerged.
Hospitals that implement continuous electronic fetal monitoring (EFM) in high-risk labors are better positioned to react rapidly. Abnormal tracings such as late decelerations, minimal variability, or bradycardia can prompt an emergency response even before maternal symptoms fully manifest.
Recommended monitoring protocols include:
| Monitoring Type | Purpose | Response Trigger |
|---|---|---|
| Fetal Heart Rate (EFM) | Detect early fetal distress | Bradycardia, prolonged decels |
| Maternal Pulse Oximetry | Spot hypoxia or sudden collapse | O2 Sat drop below 94% |
| Continuous Blood Pressure | Monitor for hypotension or shock | Sudden BP fall, especially post-pushing |
| Urine Output (Foley) | Track perfusion status | Oliguria may indicate shock onset |
ACOG guidelines recommend real-time interpretation of fetal tracings, especially during induction and instrumental delivery phases both high-risk windows for AFE.
Internal monitors like intrauterine pressure catheters (IUPC) can offer additional insight into contraction strength and uterine tone, but they come with caution. As shown in NCBI studies, their invasive nature might slightly increase the risk of maternal-fetal fluid exchange in already compromised uterine environments.
Early Intervention When Signs Appear
AFE is a sprint not a marathon. Once signs emerge, rapid intervention within minutes dramatically increases survival. That’s why facilities with standardized AFE response protocols, mock code training, and multidisciplinary readiness tend to report better outcomes.
Red flags that should immediately activate an emergency protocol include:
- Sudden drop in oxygen saturation
- Unexplained hypotension
- Seizure or altered consciousness
- Unexplained heavy vaginal bleeding
- Fetal heart rate abnormality with maternal distress
According to a multi-center cohort study on PubMed, the “Golden 5 Minutes” after symptom onset are critical. Delays in initiating CPR, administering blood products, or transferring to the OR can drastically reduce chances of maternal survival.
To improve outcomes, AFE-specific drills should be integrated into hospital staff training, mimicking real scenarios. A sample emergency protocol includes:
- Call code blue immediately
- Start high-flow oxygen and IV fluids
- Begin CPR if indicated
- Notify OB, anesthesia, blood bank
- Prepare for emergent C-section if not yet delivered
For more on the importance of timing and AFE prevention, check the internal guide on AFE causes and prevention.
Instrumental Delivery: Vacuum, Forceps, and AFE Risks
Which Instrumental Methods May Pose Higher AFE Risks
Instrumental deliveries — where tools like vacuum extractors or forceps assist the baby’s exit are sometimes necessary. But in the context of preventing Amniotic Fluid Embolism, their use needs careful consideration.
Research shows that instrumental vaginal deliveries may slightly increase the chance of trauma to the cervix or uterus, which can allow amniotic fluid to enter the maternal bloodstream. In fact, a large-scale analysis on PubMed found that vacuum and forceps deliveries were more frequent in AFE cases compared to normal deliveries.
This does not mean instrumental deliveries cause AFE, but rather that trauma-related pathways (tears, pressure, lacerations) can facilitate the entry of fetal materials into circulation a known trigger of the fatal immune reaction associated with AFE.
| Method | Invasiveness | Potential Trauma | AFE Risk Context |
|---|---|---|---|
| Forceps | High | Deep vaginal/uterine pressure | Higher trauma potential |
| Vacuum | Moderate | Scalp and perineal trauma | Slightly safer, but still risky |
| Spontaneous | None | Minimal | Lowest risk |
In most cases, forceps should be avoided in favor of vacuum or cesarean if signs of uterine scarring, poor fetal position, or maternal exhaustion are present.
For a deeper look at instrumental delivery risks, the NCBI review on operative vaginal birth complications provides comprehensive data on outcomes tied to various interventions.
Also, don’t miss the internal resource on how rare AFE is, which gives context on why prevention matters even for low-risk births.
When to Choose Cesarean Over Forceps/Vacuum
A cesarean delivery is not risk-free but in some situations, it may actually lower the risk of AFE-related complications compared to traumatic vaginal interventions. This is particularly true when:
- The fetus is in distress and quick delivery is essential
- There are signs of uterine rupture or placental abruption
- The cervix is not fully dilated but pushing is being forced
- A prior uterine surgery puts the patient at risk for tissue injury
Studies like this PubMed meta-analysis confirm that emergency cesareans, when performed quickly and with skilled teams, may reduce the severity of AFE outcomes by avoiding additional trauma and enabling rapid fetal removal.
Still, cesareans should not be overused. Elective cesareans, especially without medical need, carry their own risks including blood loss, infection, and longer recovery. The key is balancing urgency with safety, choosing the delivery route that reduces exposure to trauma and allows better response capacity if AFE occurs.
Whenever possible, delivery decisions should be discussed early in labor based on the patient’s risk profile, preferences, and the facility’s emergency capabilities.
You can find more clinical context in the internal article on pregnancy facts related to AFE.
Emergency Response Protocols and Team Preparedness
Immediate Resuscitation: What Makes the Difference
When Amniotic Fluid Embolism strikes, there is no time to hesitate. The condition evolves within minutes, causing respiratory failure, cardiac arrest, and uncontrolled bleeding. Survival depends entirely on how fast and how effectively the team reacts.
The key to improving survival is protocolized emergency response. In a NIH clinical guide, it’s clearly shown that facilities with pre-established AFE response protocols and regular staff simulation training had lower fatality rates.
Here’s a simplified AFE emergency response checklist used in top obstetric centers:
| Step | Action | Purpose |
|---|---|---|
| 1 | Call for emergency code (OB/Anesthesia) | Mobilize full team immediately |
| 2 | Secure airway + high-flow oxygen | Prevent hypoxia |
| 3 | Establish 2 large IV lines | Begin rapid fluid and blood replacement |
| 4 | Start CPR if pulseless | Maintain perfusion |
| 5 | Administer blood products + uterotonics | Manage DIC and bleeding |
| 6 | Deliver baby (if undelivered) ASAP | Improve maternal chances |
This process must begin within 3–5 minutes of symptom onset to protect both mother and baby.
Delays are often due to unclear roles, lack of drills, or limited blood bank coordination, as confirmed in this multicenter audit on PubMed.
The entire labor ward from nurses to anesthesiologists must be trained in obstetric code drills that include AFE scenarios, which mimic real-world conditions.
If the team isn’t rehearsed, confusion will cost lives. That’s the brutal reality of AFE.
Simulation Training and Hospital Readiness
In modern obstetrics, simulated emergency training is no longer optional. It’s a necessity especially for conditions like AFE, where response time equals survival.
Studies like this one from PubMed show that labor units with monthly or quarterly emergency simulations improve:
- Team coordination
- Time to diagnosis and treatment
- Confidence in performing rare protocols
- Reduction in maternal-fetal morbidity
Simulation training doesn’t only focus on physical actions it also includes verbal communication, rapid decision-making, and interdepartmental alert systems. When everyone knows their role in an AFE emergency, care becomes immediate and decisive.
Some hospital systems are now integrating AFE-specific checklists into electronic health records, ensuring that alerts automatically notify the blood bank, ICU, and surgical team if AFE is suspected.
To see a broader perspective on how protocols influence survival, visit the internal resource on pregnancy facts linked to AFE, where maternal outcomes in different clinical settings are reviewed.
Hospitals that invest in preparedness and practice save lives. It’s that simple.
Postpartum Surveillance & Long-Term Follow-Up
Why Observation Matters After Birth
Even after a baby is born, the danger of Amniotic Fluid Embolism (AFE) isn’t completely over. Some cases have been reported in the minutes or even hours following delivery, particularly during placental separation or uterine repair.
That’s why postpartum monitoring is not just routine it’s lifesaving, especially for women who had any of the known AFE triggers:
- Instrumental delivery
- Cesarean section
- Uterine rupture
- Abnormal placenta (previa or accreta)
- High-dose uterotonics
According to PubMed case studies, AFE symptoms often begin postpartum, with sudden shortness of breath, restlessness, or abnormal bleeding. These are not signs of simple exhaustion they are critical warning signs.
Best practice includes minimum 2 hours of intensive observation in a labor and delivery recovery suite, with:
| Parameter to Monitor | Why It Matters | Frequency (First 2 Hours) |
|---|---|---|
| Blood pressure | Sudden hypotension = early sign of AFE | Every 15 mins |
| Oxygen saturation | Drop signals cardiopulmonary collapse | Continuous |
| Uterine tone | Atony linked to DIC in AFE | Every 15–30 mins |
| Bleeding level | Postpartum hemorrhage = urgent action | Every 15–30 mins |
Nurses and clinicians should be trained to treat sudden maternal collapse as AFE until proven otherwise, especially if onset occurs after the third stage of labor.
To reinforce this logic, read the internal summary on how rare AFE is and why we can’t afford to ignore it, even in the recovery room.
Addressing Long-Term Maternal Impacts of AFE
Women who survive AFE face more than physical recovery. Many experience long-term complications, including:
- Cognitive changes (from lack of oxygen)
- Emotional trauma and PTSD
- Difficulty breastfeeding (due to extended ICU stays)
- Increased anxiety in future pregnancies
According to a clinical follow-up study on PubMed, survivors report feeling isolated, unheard, and anxious especially when providers dismiss their experience as “rare” and unworthy of further discussion.
Post-AFE care must include:
- Follow-up with OB/GYN and cardiology
- Mental health referral within first 30 days
- Clear discussion around future pregnancy planning
- Documentation of the event in all medical records
Most importantly, survivors should receive emotional validation and long-term monitoring not just a “you’re lucky” discharge note.
The internal article on pregnancy facts and AFE outlines common recovery issues and how to approach them with empathy and medical vigilance.
Frequently Asked Questions About Preventing AFE
What are the early warning signs of AFE during labor?
The most common first signs of Amniotic Fluid Embolism are sudden shortness of breath, confusion, panic, or a rapid drop in blood pressure. Often, fetal heart rate drops (bradycardia) appear before the mother even shows symptoms. According to a PubMed case analysis, fetal distress may be the first clue in over 80% of cases.
Can AFE be predicted through prenatal screening?
Unfortunately, no reliable test exists to predict AFE before labor. It’s considered an unpreventable and unpredictable obstetric emergency, as confirmed by the American College of Obstetricians and Gynecologists. However, identifying risk factors early (age >35, multiple gestation, placenta previa) can help plan delivery in a high-readiness hospital.
Related reading: Amniotic Fluid Embolism Risk Factors
Is there a safer induction method to lower AFE risk?
Yes. Mechanical methods (like a Foley catheter) are often safer for women at risk. Using low-dose oxytocin with continuous monitoring is preferred. Overstimulation of the uterus, especially with prostaglandins, should be avoided. See the breakdown in AFE induction strategies for more on choosing induction methods wisely.
Should high-risk women avoid vaginal delivery?
Not necessarily. Planned vaginal birth with close monitoring is often safe, but instrumental methods like forceps or vacuum should be minimized if possible. If the patient has had a previous uterine surgery or shows signs of labor complications, a cesarean may be safer, as supported in this surgical outcome review.
Does a C-section eliminate the risk of AFE?
No, but it may reduce trauma-related triggers of AFE in some high-risk patients. However, cesarean delivery has its own risks (infection, bleeding). The decision should be individualized, based on maternal health, labor progress, and facility readiness.
More details: AFE in Cesarean vs Vaginal Delivery
How quickly should a hospital respond if AFE is suspected?
Within 5 minutes. Delays beyond that reduce survival dramatically. AFE protocols must include code response, resuscitation, blood products, and possible delivery within minutes. Hospitals with routine simulation training have better outcomes, according to this PubMed study.
Conclusion
Amniotic Fluid Embolism is rare, but its impact is devastating. What makes the difference is not just treatment it’s prevention, awareness, and preparation. From carefully selecting induction methods, to being strategic with instrumental delivery, and maintaining emergency readiness, every decision matters.
This guide has explored evidence-based strategies to reduce the risk of AFE, explained in plain language for families, clinicians, and birth workers. Remember, while AFE cannot be predicted with certainty, many contributing factors are manageable, especially in properly equipped settings with trained teams.
By understanding the risks, recognizing the signs, and acting fast, we can save lives one informed birth at a time.
Don’t miss our internal analysis on amniotic fluid embolism risk factors or check out how rare AFE really is to better understand the numbers behind the fear.