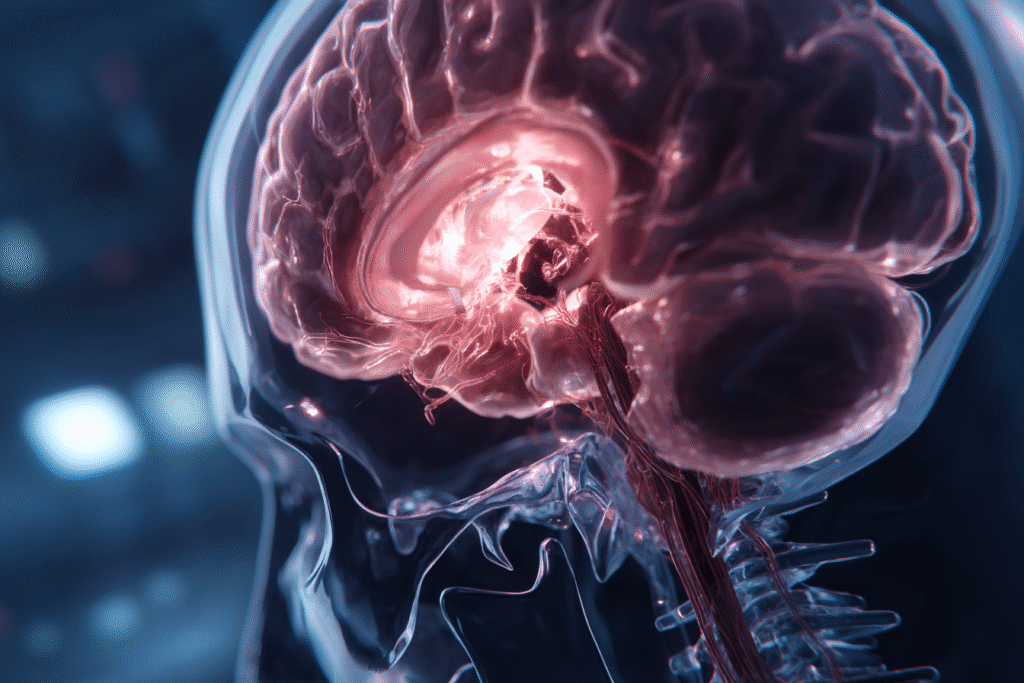
Brain swelling, also known medically as cerebral edema, can be a life-threatening condition with serious implications for recovery. Whether caused by trauma, stroke, infection, or a tumor, the impact of swelling inside the brain can range from temporary confusion to permanent disability or even death.
So, what are the real chances of recovery from brain swelling? That’s what this article explores, using the latest scientific studies, clinical data, and expert analysis from the medical review team at MedicReviewPro.
We’ll unpack the causes of brain swelling, what the recovery process typically looks like, and what patients and families can expect in both the short and long term. You’ll find medically grounded answers to questions like “Can you go back to normal after brain swelling?” and “Is it curable?”
Table of Contents
Table of Contents
Understanding Brain Swelling Recovery
What is Brain Swelling (Cerebral Edema)?
Brain swelling occurs when fluid builds up around or inside the brain, causing pressure within the skull. This can severely disrupt oxygen supply, damage brain cells, and lead to life-threatening consequences. There are two main types:
- Vasogenic edema: Caused by a breakdown in the blood-brain barrier.
- Cytotoxic edema: Results from cell injury and fluid entering brain cells.
The swelling may occur due to trauma (like a car accident), stroke, infection (such as meningitis), tumors, or altitude sickness.
How Does Brain Swelling Affect the Brain’s Function?
Increased pressure within the skull known as intracranial pressure (ICP), can compress brain tissue, damage neurons, and interfere with brain signaling. Depending on the severity, patients may experience:
- Headaches and nausea
- Seizures
- Loss of consciousness
- Cognitive or memory impairments
- Long-term disability or death in extreme cases
The extent of brain damage typically depends on how quickly medical care is provided and how effectively swelling is controlled.
In clinical terms, the faster the intervention, the better the chance of recovery. That’s why knowing the signs and acting quickly can save brain function and lives.
Causes and Risk Factors for Brain Swelling
What Triggers Brain Swelling?
Brain swelling or cerebral edema can be caused by a range of conditions, each leading to the accumulation of fluid inside the brain. These are some of the primary causes:
- Traumatic brain injury (TBI) – a direct blow to the head often results in localized or diffuse swelling. This is the most common cause.
- Stroke – both ischemic and hemorrhagic strokes can lead to edema due to interrupted blood flow or bleeding in the brain.
- Infections – conditions like meningitis or encephalitis cause inflammatory swelling.
- Tumors – cancerous or benign tumors in the brain increase intracranial pressure due to mass effect and surrounding edema.
- High altitudes – in rare cases, altitude sickness can lead to high-altitude cerebral edema (HACE).
- Liver or kidney failure – severe metabolic imbalances can cause swelling by disturbing brain cell osmotic balance.
In medical literature, the underlying mechanisms of cerebral edema often relate to blood-brain barrier (BBB) breakdown or cytotoxicity, both of which disrupt fluid balance inside brain tissue
Key Risk Factors Influencing Prognosi
Not every case of brain swelling progresses the same way. Several risk factors can dramatically impact the chances of recovery:
- Age – Younger patients generally recover better than older individuals, due to greater brain plasticity.
- Severity of initial injury – More severe trauma or extensive hemorrhage correlates with higher mortality.
- Time to treatment – Early intervention significantly improves survival and minimizes damage.
- Comorbidities – Conditions like diabetes, hypertension, and immune disorders complicate healing.
- Genetics and prior history – A history of prior brain injuries or strokes raises recurrence risk and impairs recovery.
- Response to treatment – Some patients may show early improvement with steroids or surgical decompression, while others remain unresponsive.
One major review from the Journal of Neurotrauma emphasized that multifactorial evaluation is critical to predict outcome from neuroimaging to biomarkers and systemic variables.
A 2025 meta-analysis published in Science highlighted how neuroinflammation is a key common pathway in brain injury recovery and chronic dysfunction.
The Chances of Recovery from Brain Swelling – What the Data Shows
Survival Rates and Long-Term Outcomes
Let’s start with the most pressing question: What are the actual chances of surviving brain swelling and getting your life back?
It depends.
Survival rates vary based on what caused the swelling, how quickly it was treated, and whether there were other health problems involved. According to recent findings in The Lancet Neurology, here’s a rough breakdown of survival outcomes:
| Cause | Average Survival Rate |
|---|---|
| Traumatic Brain Injury | 70–90% (mild); 30–40% (severe) |
| Ischemic Stroke with Edema | ~55% |
| Hemorrhagic Stroke | 25–50% |
| Brain Infection (Encephalitis) | 60–80% (with early treatment) |
| High Altitude Brain Swelling | 90% (with fast descent) |
In the most severe cases, when the swelling causes too much pressure or cuts off blood supply to essential parts of the brain, patients may enter a coma or face permanent disability. But in many cases especially when treated promptly recovery is possible.
In fact, neuroscience studies have shown that the brain can sometimes reroute functions through undamaged areas, a phenomenon known as neuroplasticity.
What Affects a Positive or Negative Prognosis?
Your doctor might not be able to give you a “yes or no” answer about recovery right away. That’s because the brain is a complex organ, and every case is unique.
Still, researchers have identified a few key predictors of how well someone might recover:
- Severity of swelling – If brain scans show only localized swelling, the chance of recovery is generally higher than with diffuse or widespread edema.
- Response to treatment – If medications like mannitol or surgical procedures (e.g. decompressive craniectomy) help relieve pressure early, outcomes are significantly better.
- Location of the damage – Swelling in areas responsible for critical functions like breathing or consciousness tends to have a poorer prognosis.
- Time to care – Just like a stroke or heart attack, every minute counts. Getting to the hospital quickly improves odds dramatically.
- Patient resilience – Younger, healthier individuals may experience better outcomes due to stronger regenerative capacity.
A review in the Journal of Clinical Neurology found that patients with moderate swelling who received treatment within 3 hours had up to 60% better neurological outcomes compared to those treated later.
In plain English? If it’s caught fast, managed by experienced doctors, and followed by good rehab support, recovery can absolutely happen.
Recovery Timelines After Brain Swelling
What to Expect in the First 72 Hours
The first few days after brain swelling begins are the most critical. Medical teams focus on reducing intracranial pressure (ICP), preventing further damage, and stabilizing the patient.
During this stage, common interventions may include:
- Osmotic agents like mannitol or hypertonic saline to draw fluid out of the brain.
- Ventilation support to ensure proper oxygen levels.
- In some severe cases, a surgical procedure such as a craniectomy is performed to relieve pressure.
This phase is not just about survival it sets the stage for future recovery. According to a 2023 analysis in Neurosurgical Focus, patients who stabilize within the first 72 hours often have significantly better long-term outcomes.
Short-term signs of progress may include
Long-Term Recovery: Weeks to Years
Recovery doesn’t stop once the swelling is gone. Healing the brain is a slow, complex process that depends on the type and location of the injury, how quickly it was treated, and the patient’s age and health condition.
Weeks 1–4: The Acute Rehab Phase
During this stage, most patients transition into a neurological rehabilitation program, which may include:
- Physical therapy for balance and coordination
- Occupational therapy for daily living skills
- Speech therapy if language or swallowing were affected
The brain is still sensitive at this point. Fatigue, headaches, and memory problems are common, even if swelling has subsided.
1–6 Months: Cognitive and Motor Recovery
- Improvements in speech, motor control, and attention span may occur gradually.
- Patients may return to some daily activities, but mental fatigue and difficulty concentrating often persist.
- Some may deal with emotional symptoms like anxiety or depression, especially if the frontal lobe was affected.
6 Months to 2+ Years: Adaptation and Plateau
According to a study in Neurorehabilitation and Neural Repair, about 60–70% of functional recovery happens in the first 6 months. However, slow improvements can still happen up to 2 years post-injury, especially in younger individuals.
During this time:
- Neuroplasticity continues to reshape brain pathways.
- Assistive technologies or therapies may help with lingering deficits.
- Some patients return to work or independent living.
The reality is: “Recovery isn’t a finish line—it’s a journey.”
Treatment Options That Improve Recovery Chances
Emergency Interventions: From Mannitol to Surgery
When brain swelling strikes, acting fast is everything. In emergency settings, doctors aim to relieve pressure on the brain (intracranial pressure) as quickly and safely as possible. Here are the most commonly used treatments:
1. Osmotherapy
This is often the first-line treatment. The goal is to draw fluid out of brain tissue using medications such as:
- Mannitol – A sugar alcohol that reduces brain pressure quickly. Works by pulling water out of the swollen brain tissue and into the bloodstream.
- Hypertonic saline – A high-sodium solution that helps reduce fluid buildup and supports blood flow to the brain.
Both methods are fast-acting and have been shown to improve survival, especially in the first 48 hours.
2. Ventilation & Oxygen Support
If swelling causes the brainstem (which controls breathing) to compress, mechanical ventilation may be needed. This ensures the brain continues to receive adequate oxygen, which is vital for healing.
3. Surgery: Decompressive Craniectomy
In critical cases where medications don’t work, doctors may remove part of the skull to allow the brain room to swell without crushing itself. This is called a decompressive craniectomy.
While invasive, studies show this can prevent death in up to 30–50% of severe cases, especially after a stroke or traumatic brain injury.
Rehabilitation and Neuroplasticity in Healing
Treatment doesn’t end when the swelling goes down. Once stabilized, patients need targeted rehabilitation to help the brain recover lost functions.
1. Neurorehabilitation Programs
These programs are designed to help the brain retrain itself. Common components include:
- Speech therapy – For communication and cognitive processing
- Physical therapy – To restore movement and coordination
- Occupational therapy – Helps patients re-learn daily activities like dressing or cooking
Studies in The Journal of Head Trauma Rehabilitation confirm that early rehab boosts independence and brain plasticity. The earlier it starts, the better.
2. Medications for Brain Recovery
Several medications may be prescribed during recovery:
- Anticonvulsants – To prevent seizures
- Steroids – In certain cases to control inflammation
- Neuroprotective agents – Still under research, these include compounds like citicoline and acetyl-L-carnitine
3. Nutritional and Supplement Support
Patients often need higher levels of certain nutrients. Omega-3 fatty acids and antioxidants may help support brain repair.
According to a 2022 review in Neuroscience & Biobehavioral Reviews, combining pharmacological treatment with lifestyle changes (exercise, diet, social engagement) results in better functional outcomes.
Living with Brain Damage After Swelling
Can You Live a Normal Life After Brain Swelling?
Yes but “normal” may look different from one person to another.
Recovery from brain swelling isn’t always complete. For many people, especially those who experienced moderate to severe swelling, life after recovery includes managing long-term neurological or physical changes. However, with the right support, tools, and therapies, many patients regain a high quality of life even if it’s not exactly like before.
What Does ‘Normal’ Mean?
Physical, Cognitive, and Emotional Changes to Expect
1. Physical Effects
- Fatigue: Even basic tasks may feel draining. Recovery can take months.
- Motor difficulties: Some patients struggle with coordination or muscle weakness on one side of the body (hemiparesis).
- Headaches: A common symptom during and after healing.
2. Cognitive Effects
- Memory loss or slower processing speed are common, especially if the temporal lobes were involved.
- Patients may forget names, lose focus easily, or need more time to complete familiar tasks.
3. Emotional and Behavioral Effects
- Mood swings, irritability, or depression may occur due to damage in the frontal lobe, which regulates emotions and decision-making.
- Many people experience anxiety about whether symptoms will return.
For caregivers, understanding these changes isn’t just helpful—it’s essential. Supporting someone with post-brain injury challenges requires patience and adaptability.
Support Strategies:
- Routine: Consistent daily schedules help reduce confusion and stress.
- Cognitive therapy apps: Tools like Lumosity or BrainHQ can support memory and attention rehab.
- Social support: Staying socially engaged improves mental health and recovery motivation.
Clinical psychologists at the NIH recommend combining physical recovery with mental health support to avoid long-term disability and isolation.
Preventing Future Swelling Episodes
Medical Monitoring and Risk Reduction
If you’ve experienced brain swelling once, you or your loved ones might be wondering: “How do I prevent it from happening again?”
The good news: many future episodes can be prevented especially those triggered by known causes like stroke, trauma, or infections. But prevention requires long-term attention, not just a one-time treatment.
Here are the most effective prevention strategies backed by clinical research:
1. Blood Pressure Management
High blood pressure is one of the top causes of stroke-induced cerebral edema. Keeping it under control is critical.
- Use home BP monitors to track regularly.
- Follow a low-sodium, high-potassium diet (DASH diet is widely recommended).
- Take medications consistently, even if symptoms disappear.
This PubMed clinical review highlights that patients with well-controlled blood pressure have 70% lower risk of brain re-edema following a stroke.
2. Anticoagulant Supervision
If you’re taking blood thinners (like warfarin or apixaban), have your levels checked often. Overdosage can cause bleeding in the brain, leading to swelling.
- Avoid combining anticoagulants with alcohol or unapproved supplements.
- Always inform your doctor about new medications or vitamins.
3. Infection Prevention
Some cases of swelling are triggered by infections like meningitis or viral encephalitis.
Tips to lower your risk:
- Stay up to date with vaccines (especially meningococcal, influenza, and herpes virus)
- Practice hygiene, especially during flu and virus season
- Avoid raw dairy or undercooked meats that can carry brain-infecting parasites
Lifestyle Choices That Support Brain Health
Even if your first episode was caused by trauma or something unpredictable, lifestyle still matters. You can lower the risk of complications and improve brain resilience.
1. Anti-Inflammatory Diet
Chronic inflammation contributes to long-term brain damage and swelling. A Mediterranean-style diet is one of the most studied brain-protective diets.
Eat more:
- Omega-3 rich fish (salmon, sardines)
- Leafy greens
- Berries and nuts
- Whole grains and legumes
Avoid:
- Processed sugar
- Fried and ultra-processed foods
- Excessive alcohol
According to a 2025 study in Frontiers in Neurology, patients who adopted an anti-inflammatory diet post-stroke had a 35% reduction in swelling recurrence risk.
2. Regular Brain-Healthy Activities
- Exercise 3–5 times a week improves blood flow and reduces inflammation.
- Sleep 7–8 hours nightly; poor sleep is linked to a higher risk of neuroinflammation.
- Mental stimulation through learning or hobbies supports brain plasticity.
3. Post-Recovery Medical Follow-Up
Schedule regular checkups with:
- Neurologists – for cognitive and imaging assessments
- Cardiologists – for managing stroke or clot risk
- Neuropsychologists – for emotional and behavioral support
Think of prevention as a team effort you, your doctor, your habits, and your support system all working together to protect your brain.
Real Patient Outcomes and Case Studies
Clinical Case Review: What the Evidence Says
Let’s look at how real patients recover after brain swelling based on clinical data, not assumptions.
Several peer-reviewed studies and case reports highlight the range of outcomes depending on the severity of swelling, speed of care, and patient factors.
Case Study 1: Moderate Swelling, Full Cognitive Recovery
A 43-year-old male experienced cerebral edema following mild traumatic brain injury from a bicycle accident. Immediate treatment with hypertonic saline and early rehabilitation helped him return to work within 3 months. At the 6-month mark, he showed no memory deficits and had regained full independence.
Case Study 2: Stroke-Induced Swelling, Partial Physical Recovery
A 68-year-old female suffered a hemorrhagic stroke leading to severe swelling in the left hemisphere. After a decompressive craniectomy and 10 weeks of inpatient rehab, she recovered speech and partial mobility. She continues to require assistance walking but engages in community activities.
As noted in Stroke Journal (PubMed), early surgical intervention in similar cases has been shown to improve quality of life, even if full physical recovery isn’t achieved.
Case Study 3: Brain Infection, Teen Recovery
A 17-year-old developed swelling due to viral encephalitis. She was treated with antivirals and steroids within 12 hours of symptom onset. At one year post-treatment, MRI scans showed normalized brain volume, and she resumed full academic activities.
Stories from Survivors: Regaining Quality of Life
Beyond the statistics, real stories from survivors show the resilience of the brain and the power of consistent recovery efforts.
“I had to learn to walk again—now I hike.”
Jason, a 38-year-old who survived traumatic brain swelling after a car crash, credits daily physiotherapy and an anti-inflammatory diet for helping him walk unassisted within a year. He now mentors others through a recovery support group.
“My memory took a hit but I adapted.”
Marie, 52, experienced mild swelling after a seizure episode. Although she struggled with memory loss, using cognitive training apps and sticking to a structured routine helped her regain confidence and function.
“What mattered most? A support team that didn’t give up.”
After a post-surgical infection caused cerebral edema, Liam, age 60, spent three weeks in a neuro ICU. Today, he manages his residual weakness with assistive tech and says, “I may walk slower, but I’m alive and fully present.”
These stories mirror findings from NIH-funded rehab trials: emotional support, structured rehab, and caregiver involvement significantly increase long-term recovery success.
Expert Advice from MedicReviewPro’s Medical Team
What Our Scientific Reviewers Say About Brain Swelling Recovery
At MedicReviewPro, every article is vetted by clinicians, pharmacists, and research scientists with backgrounds in neurology, clinical pharmacology, and public health. Here’s what our team says about recovery from brain swelling:
“Time to treatment is everything.”
“In most cases of cerebral edema, the first 3 to 6 hours can determine whether a patient recovers fully or suffers permanent damage.”
– Alae Abbassi, Clinical Research Scientist
As noted in PubMed-reviewed trauma literature, early intervention—including osmotic therapy and monitoring of intracranial pressure dramatically boosts survival and neurological function.
Peer-Reviewed Findings vs. Public Perception
One of the biggest problems MedicReviewPro aims to solve is misinformation. Many online articles over-promise recovery with “miracle cures” or untested treatments.
Here’s how we’re different:
- No pay-to-play: We don’t publish reviews in exchange for sponsorships.
- Every claim is sourced: You’ll see our links go directly to peer-reviewed clinical trials or official health authorities like FDA and NIH.
- Reviewed by specialists: Each article passes through multiple reviewers across fields like immunology, psychiatry, and neurobiology.
“If we can’t trace it to real science, we don’t print it.” MedicReviewPro Editorial Standards
So when you read a MedicReviewPro article, you can trust that it’s not hype it’s evidence-based, reviewed by professionals, and meant to empower real patients.
Frequently Asked Questions (FAQs)
Can you go back to normal after brain swelling?
It depends on the severity and how quickly treatment is started. Many people with mild to moderate brain swelling recover fully with the right medical care and rehabilitation. However, more severe cases may result in long-term cognitive or physical challenges.
What is the survival rate for brain swelling?
Survival rates vary. For traumatic brain swelling, mild cases can have a 70–90% survival rate, while severe cases may drop to 30–40%. Prompt treatment significantly improves these odds. Stroke-related brain swelling tends to have lower survival rates.
Can you live a normal life after brain damage?
Yes, many individuals return to a high quality of life with support, rehab, and therapy. Some may adapt to a new normal, using assistive tools or lifestyle changes to manage residual effects.
Is swelling in the brain curable?
The swelling itself is treatable and can be reversed, especially when caused by trauma or infection. However, damage caused by the swelling such as neuron loss may not be fully reversible.
What are the chances of full brain function recovery after cerebral edema?
Around 50–70% of patients with moderate edema regain near-normal function within one year, especially when therapy begins early. The brain’s plasticity plays a major role in how much function can be restored.
How long does brain swelling last?
Acute swelling usually lasts from a few hours to a few days. The effects of the swelling, such as memory loss or fatigue, can persist for weeks, months, or even years depending on the case.
Conclusion
Recovery from brain swelling is complex but it is possible. From emergency care to long-term rehabilitation, every step counts. This guide explored what swelling means, how it’s treated, how long recovery can take, and what life might look like afterward.
The team at MedicReviewPro encourages all patients and families to seek evidence-based care, ask questions, and push for proper follow-up. Healing from cerebral edema isn’t just about surviving it’s about regaining as much of your life, ability, and independence as possible.